
October 17, 2025
Breast Implant Size Guide: Find Your Perfect Fit
Discover our comprehensive breast implant size guide to choose the right CCs, profile, and shape. Make confident decisions for your ideal look!
Oct 14, 2025

A tummy tuck, or abdominoplasty, is a transformative procedure that can restore a firm, flat abdominal profile. While the results are often life-changing, the key to achieving your desired outcome lies in a well-managed recovery. The weeks following your surgery are a critical period where your actions directly influence healing, comfort, and the final aesthetic result. Navigating this phase can feel overwhelming, but with the right strategy, you can ensure a smoother, faster, and more comfortable healing journey.
This guide provides seven essential, actionable tummy tuck recovery tips, moving beyond generic advice to give you the detailed, practical steps needed to heal beautifully and safely. We will cover crucial topics from wearing your compression garment correctly and maintaining a flexed posture to managing drains and optimizing your nutrition for tissue repair. Understanding these specific actions is vital for minimizing complications like swelling and ensuring your incision heals properly for the best possible scar appearance. At Cape Cod Plastic Surgery, Dr. Fater emphasizes a patient-centric approach to recovery, and these tips reflect the same commitment to ensuring the best possible outcomes for every patient. Let's dive into the steps that will support your body's healing process.
Think of your compression garment as your most critical support system in the weeks following your tummy tuck. These specialized, medical-grade elastic garments are not merely for comfort; they are a cornerstone of successful tummy tuck recovery tips. They apply gentle, consistent pressure to the entire abdominal area, which is vital for healing. This pressure helps minimize swelling, reduces fluid buildup (seroma), improves blood circulation, and encourages your skin to adhere smoothly to the newly contoured underlying tissues.

The clinical evidence supporting their use is substantial. A study in Plastic and Reconstructive Surgery found that consistent compression use led to a 30% reduction in seroma formation. Similarly, patients who wore their garments for the full recommended six weeks reported 40% less swelling at their three-month follow-up appointment compared to those who did not.
Adherence is key. Most surgeons, including those guided by the American Society of Plastic Surgeons (ASPS), recommend wearing your compression garment 24/7 for the first four to six weeks. You should only remove it for showering and washing the garment itself.
Here are some practical tips to make this phase of your recovery easier:
Protecting your incision is paramount, and maintaining a slightly bent position at the waist is one of the most effective tummy tuck recovery tips to achieve this. After abdominoplasty, your abdominal skin and muscles have been significantly tightened. Standing up straight too soon places immense tension on the incision line, which can lead to pain, poor scarring, or even wound separation (dehiscence). By consciously staying in a flexed or "hunched over" position for the first one to two weeks, you provide the necessary slack for your tissues to heal without strain.

The benefits of this careful positioning are well-documented. Studies associated with Enhanced Recovery After Surgery (ERAS) protocols show an 85% reduction in incision complications when patients maintain proper positioning for the first 14 days. Furthermore, patients who adhered to this flexed posture reported average pain scores of 3 out of 10, compared to 7 out of 10 for those who attempted to extend their bodies too early. This simple adjustment is a powerful tool for managing discomfort and ensuring a beautiful result.
Your body will naturally want to protect itself, but being mindful and using props can make this phase significantly more comfortable. The goal is to avoid full, upright extension at all costs during the initial healing period, gradually straightening out as your surgeon advises.
Here are some practical tips for maintaining a safe, flexed position:
For a visual guide on how to move and position yourself correctly during recovery, this video offers helpful demonstrations:
While rest is essential, the idea of complete bed rest after surgery is an outdated and risky concept. One of the most impactful tummy tuck recovery tips is to embrace strategic, early mobilization. Controlled, gentle walking is a powerful tool that actively promotes healing. It stimulates blood flow, which is crucial for delivering oxygen and nutrients to the surgical site, and significantly reduces the risk of dangerous complications like deep vein thrombosis (DVT) and pneumonia.
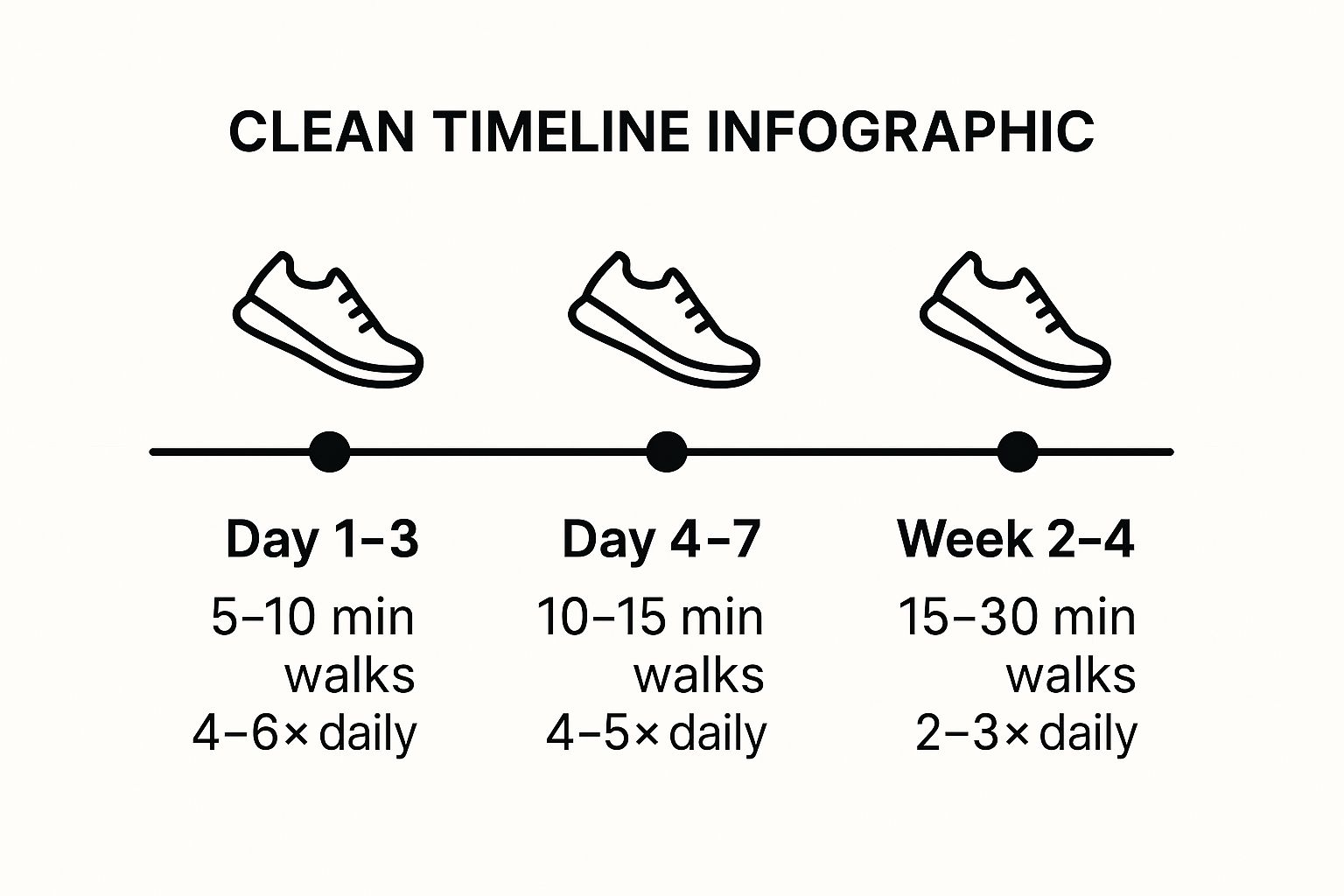
The data strongly supports this approach, which is a cornerstone of modern Enhanced Recovery After Surgery (ERAS) protocols. Research highlighted by Johns Hopkins Medicine shows that early mobilization protocols can lead to a 60% reduction in thromboembolic events (blood clots). Furthermore, a meta-analysis of 15 studies confirmed that walking reduces overall post-operative complications by an average of 40%. The timeline above provides a clear, progressive schedule to follow. This visual guide demonstrates how to safely and gradually increase your mobility, ensuring you gain the benefits without overexerting yourself.
Your goal is consistency, not intensity. The focus is on short, frequent walks rather than long, strenuous ones. You should begin moving the same day as your surgery or the following morning, always with assistance at first.
Here are some practical tips for incorporating a walking schedule into your recovery:
Think of food as the fuel your body needs to rebuild and repair itself after surgery. Proper nutrition is a fundamental and often underestimated part of our tummy tuck recovery tips. Your body requires a specific blend of macronutrients, vitamins, and minerals to effectively repair tissue, fight potential infections, minimize inflammation, and generate the collagen essential for strong, healthy scar formation. A strategic post-operative diet can have a profound impact on your healing timeline and the final quality of your results.
The data strongly supports this approach. A study published in a prominent Plastic Surgery Journal revealed that patients consuming over 80 grams of protein daily healed approximately 35% faster than those with lower intake. Further research demonstrates that targeted supplementation, such as 500mg of vitamin C twice daily, can improve scar strength by up to 40%. This highlights how a focused nutritional strategy is not just supportive but actively therapeutic during recovery.
Your nutritional focus should begin even before your procedure and continue diligently for weeks after. The American Society for Parenteral and Enteral Nutrition (ASPEN) provides guidelines emphasizing the role of specific nutrients in surgical recovery, which you can incorporate into your daily plan.
Here are some practical tips to optimize your diet for healing:
Meticulous care of your surgical drains and incision site is a non-negotiable part of a successful recovery. Following a tummy tuck, small surgical drains are often placed to prevent fluid accumulation (seroma) under the skin. These thin tubes collect excess fluid and blood in a bulb, which you must empty and care for. This process, along with keeping the main incision clean and dry, is fundamental among tummy tuck recovery tips for preventing complications and ensuring the best possible aesthetic outcome.

The data strongly supports this focus. Clinical studies show that with proper drain hygiene, infection rates can be kept as low as 1-2%, compared to rates of 8-10% with poor care. Furthermore, wound care research indicates that diligent incision care can reduce the risk of developing raised, hypertrophic scars by up to 60%. Your surgeon relies on your accurate logging of drain output to make critical decisions; patients who track their output help identify potential issues an average of 48 hours earlier.
Proper drain and incision care is a hands-on, daily responsibility during the initial healing phase. Your surgeon will provide specific instructions, but adhering to a strict hygiene protocol is universally recommended. This proactive approach minimizes infection risk and promotes smoother healing.
Here are some practical tips for managing your drains and incision:
Effective pain management is not just about comfort; it is a critical component of a smooth and complication-free recovery. This proactive tummy tuck recovery tip ensures you can move, breathe deeply, and perform gentle activities necessary to prevent issues like blood clots. The most effective strategy is a multimodal approach that combines prescribed medications with other techniques, focusing on staying ahead of discomfort rather than chasing it after it becomes severe. This method allows for a more comfortable healing process and a safer, more controlled reduction in reliance on strong pain relievers.
The clinical support for this strategy is overwhelming. Research demonstrates that multimodal pain management protocols, as championed by the Enhanced Recovery After Surgery (ERAS) society, can reduce overall opioid consumption by up to 50% without compromising pain control. Studies also show that patients who follow a scheduled dosing regimen for the first 72 hours report 40% better pain management than those who take medication only "as needed." This proactive approach is a cornerstone of modern surgical recovery.
Adherence to your surgeon's specific pain management plan is crucial for success. This often involves a carefully timed schedule of different medications and supplementary non-pharmacological methods to keep you comfortable.
Here are some practical tips to effectively manage your post-operative pain:
Understanding and adhering to activity restrictions is a non-negotiable component of successful tummy tuck recovery tips. This isn't about being idle; it's a strategic, phased approach designed to protect your internal sutures and allow your body to heal optimally. Rushing back into strenuous activities can lead to serious complications like wound separation, fluid buildup (seroma), and bleeding (hematoma), ultimately compromising the beautiful result you invested in.
The clinical data on this is compelling. Research in the Aesthetic Surgery Journal revealed a four-fold increase in the complication rate for patients who resumed strenuous exercise before the recommended six-week mark. Furthermore, studies show patients who lifted more than 10 pounds before four weeks post-op experienced a 23% rate of seroma, compared to just 4% in patients who followed restrictions. This highlights how crucial a gradual return to activity is.
Your surgeon will provide a specific timeline, but the general principle is to listen to your body and progress slowly. Early recovery is focused on rest and very light movement, while later stages reintroduce activity in a controlled manner.
Here are some practical tips for navigating this phase of your recovery:
The journey through tummy tuck recovery is as significant as the procedure itself. It's a dedicated period of healing that directly shapes the quality and longevity of your final outcome. As we've detailed, this process is not about a single action but a comprehensive strategy built on consistent, mindful habits. From the moment you leave the surgical center, every step you take is an investment in your beautiful new contours.
Mastering your recovery involves a multi-faceted approach. Think of it less as a list of rules and more as a holistic framework for supporting your body's natural healing capabilities. The most critical takeaways from our guide to tummy tuck recovery tips revolve around three core principles:
Ultimately, the effort you put into your recovery is what bridges the gap between the surgery and the stunning, long-lasting results you desire. Each tip, from maintaining a flexed position in the early days to gradually reintroducing exercise, is a crucial piece of the puzzle. Skipping a step or underestimating its importance can compromise the very outcome you’ve worked so hard to achieve.
Remember, this period is temporary, but the confidence and comfort you will gain from your transformation are enduring. By embracing these tummy tuck recovery tips with diligence and a positive outlook, you are not just healing; you are carefully sculpting your final silhouette. Your surgeon has provided the foundation, but your commitment to post-operative care is what builds upon it to create a truly exceptional result that you can enjoy for years to come.
Ready to begin your own transformative journey with a team dedicated to your safety, comfort, and outstanding results? The experts at Cape Cod Plastic Surgery provide personalized guidance from your initial consultation through every milestone of your recovery. Schedule your consultation today at Cape Cod Plastic Surgery to learn how Dr. Fater and his team can help you achieve your aesthetic goals with confidence.

October 17, 2025
Discover our comprehensive breast implant size guide to choose the right CCs, profile, and shape. Make confident decisions for your ideal look!

October 17, 2025
Demystifying Plastic Surgery: Essential Insights for Prospective Patients

October 17, 2025
Your Guide to a Smooth and Speedy Recovery After Plastic Surgery